At the Forefront of Health Care and Health Equity with Innovative Therapeutics and Diagnostics
Introduction
Notable advancements in drug discovery from researchers across the university’s health enterprise leverage technological advancements and traditional exchanges with collaborative institutions across the country to lead the way new medicine is developed and delivered.
Novel Cancer Drug Holds Promise to Fill Gap in Treatment

Researchers from the University of Illinois Cancer Center have unveiled the remarkable potential of a novel drug called PAC-1 in combating a wide range of cancers, with minimal side effects, according to Phase I clinical trials. PAC-1 has demonstrated impressive results in halting tumor growth and reducing tumor size in patients with neuroendocrine cancer. Its therapeutic activity against sarcoma has also been confirmed in the British Journal of Cancer. This trial, along with another trial examining the effectiveness of PAC-1 against brain cancer, is a collaborative effort between UIC, Johns Hopkins and Regions Hospital in St. Paul, Minnesota.
The Phase I process, as described by Oana Danciu, MD, associate professor of medicine in the department of medicine’s division of hematology and oncology, begins with extremely low doses of the drug while monitoring side effects. Over several months, providing no dangerous toxicity occurs, the dose is gradually increased until the potentially therapeutic amount is reached.
The research team remains optimistic over PAC-1’s promising results affecting neuroendocrine tumors, a type of abnormality that is lacking comprehensive drug treatment options. More insights from the Phase I clinical trial involving the potential of PAC-1 to treat glioblastoma multiforme, an aggressive brain cancer type, are also on the horizon.
Researchers Discover Mechanism to Make Leukemia Treatment Safer
Also, related to the field of oncology, College of Medicine researchers, collaborating with partners at the University of Arizona, the University of Pennsylvania and the Chinese University of Hong Kong have discovered the mechanisms that cause the leukemia drug ponatinib to harm the heart, leading to potentially fatal heart failure. The researchers were interested in understanding the interaction between ponatinib and the heart cells responsible for contraction. They discovered that ponatinib damages these cells by activating a process known as the integrated stress response.
To see if this response was harming the cells, the researchers studied what would happen if they used a small molecule to block the integrated stress response in both cells and in mice during ponatinib treatment. Findings indicate that the treatment helped protect heart cells from the damaging side effects of the drug yet did not diminish ponatinib’s tumor-fighting efficacy. “It protects the heart, but at the same time, it still allows us to kill cancer cells,” said Dr. Sang Ging Ong, assistant professor of pharmacology and medicine and senior author of the study. The study is part of a growing field called cardio-oncology that investigates drugs that shrink tumors but can also cause heart problems.
New Vaccine in Development to Treat Mosquito-borne Disease

A vaccine is being developed at the College of Medicine Rockford to protect millions of people at risk for a debilitating mosquito-borne disease is moving closer to becoming available thanks to a three-year grant totaling $2.4 million from the National Institutes of Health. Ramaswamy Kalyanasundaram, DVM, PhD, professor and head of the department of biomedical science at the College of Medicine Rockford, working with PAI Life Sciences, a biotechnology company in Seattle specializing in translational research for neglected tropical diseases, received the three-year NIH Small Business Innovation Research Phase IIB grant. The grant will allow completion of pre-Investigative New Drug studies in order to obtain FDA approval to start the human clinical trial of the first human lymphatic filariasis vaccine.
Lymphatic filariasis is a mosquito-transmitted disease caused by three filarial parasites. According to the CDC, lymphatic filariasis is a leading cause of permanent disability worldwide. Affected people frequently are unable to work because of their disability, and this harms their families and their communities. According to the World Health Organization, more than 51 million people are currently infected and another 882 million people in 44 countries are at risk of acquiring the infection – so an effective control strategy such as a vaccine is needed.
Novel Gene Therapy Approved for Treatment of Sickle Cell Disease
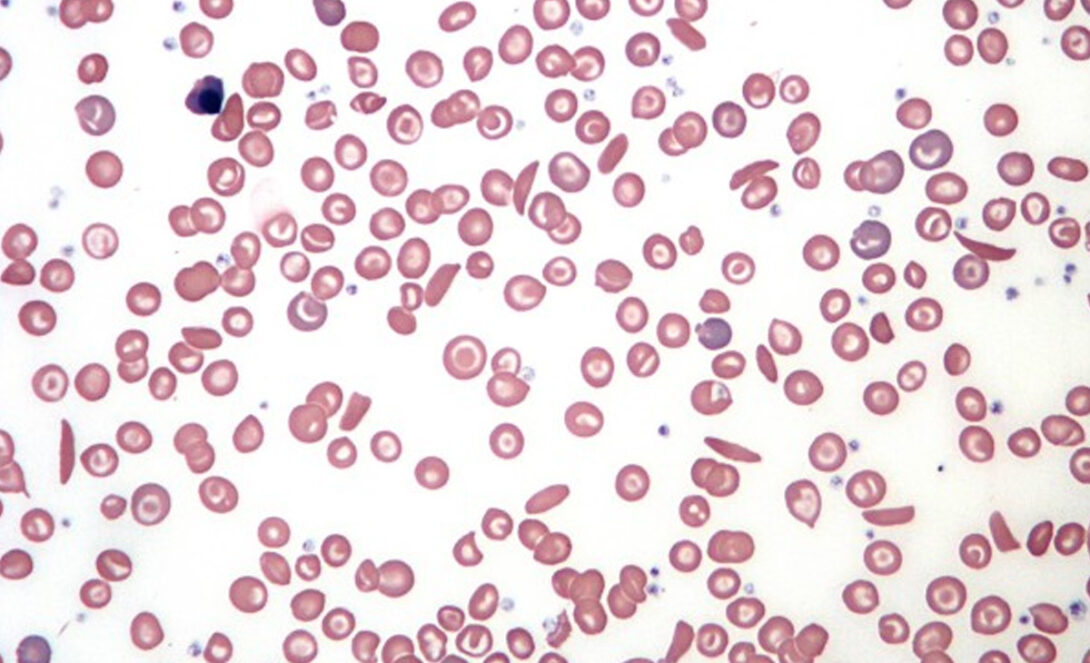
In more news from UI Health, regulators recently approved a groundbreaking protocol that has the potential to relieve some of the 100,000 Americans, most of them Black, who suffer from chronic sickle cell disease. UIC has joined 10 other medical institutions including the University of Chicago to use this treatment. UI Health, UIC’s academic healthcare enterprise, has around 600 sickle patients – among the largest such programs in the nation. Sickle cell causes not only debilitating pain, but also anemia, organ damage, strokes and, often, an early death.
The new treatment alters patients’ genes to produce healthy round red blood cells, rather than the crescent- or sickle-shaped cells that cause the disease. It is the first therapy approved by the U.S. Food and Drug Administration to use CRISPR/Cas9 gene therapy. CRISPR is a revolutionary tool that can cut and remove, add or replace DNA in targeted areas to address different genetic disorders.
At UIC, Dr. Damiano Rondelli, MD, Michael Reese professor of hematology, chief of the division of hematology and oncology and director of blood & marrow transplant in the in the College of Medicine, coauthored a study showing how gene therapy helped patients with sickle cell disease. While gene therapy carries unknown long-term effects and potential risks, such as allergic reactions or tissue damage, Dr. Rondelli said both donated transplants, which has been the standard treatment to date, and gene therapy can give patients freedom to live. One donor recipient began searching for a home to buy now that he was finally healthier. “Patients find a new life they never knew they could have,” Dr. Rondelli said.
New Brush Biopsy Will Revolutionize Diagnosis of Oral Cancer

Researchers in the College of Dentistry have developed a revolutionary diagnostic tool that can detect the most common form of oral cancer using a simple brush. The new method, known as brush biopsy, improves upon the current standard of surgical biopsies, which can often lose patients who don’t return for follow-up appointments. This new screening method, which is currently seeking commercialization partnerships, improves upon the current diagnostic standard of surgical biopsies — an extra referral step that risks losing patients who sometimes don’t return until the cancer progresses to more advanced, hard-to-treat stages.
“So many patients get lost; they don’t follow up,” said Joel Schwartz, DMD, DMedSc, and co-inventor of the brush biopsy along with Guy Adami, PhD. Both are professors in the department of Oral Medicine and Diagnostic Sciences. “We’ve tried to keep our focus mainly on early Stage 1 and 2 cancers, so it actually works with the cancers that you want to detect,” said Dr. Schwartz.
Drs. Schwartz and Adami hope that the new test will make screening easier to perform, particularly within patient populations that don’t receive regular dental care or have a higher incidence of oral squamous cell carcinoma. For example, Black men have a dramatically lower survival rate with the disease compared with white, Hispanic and Asian men. Usage of the invention in nonclinical settings would allow earlier cancer detection in high-risk populations. The work was supported by grants from the National Science Foundation and the National Cancer Institute.
Novel Laboratory Model Will Advance Our Understanding of Atrial Fibrillation
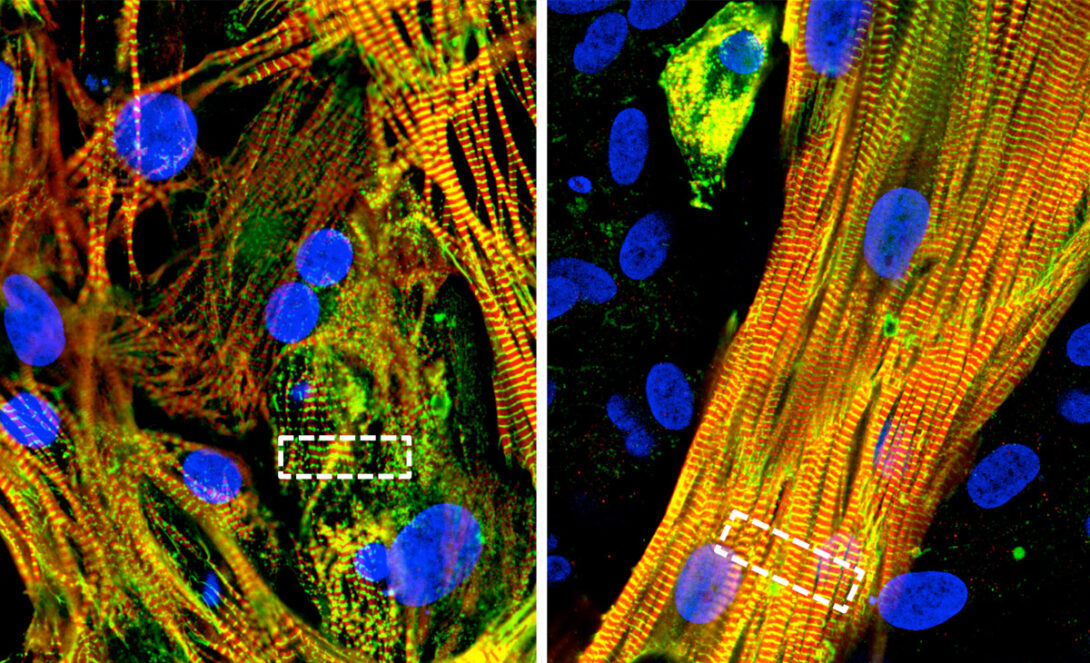
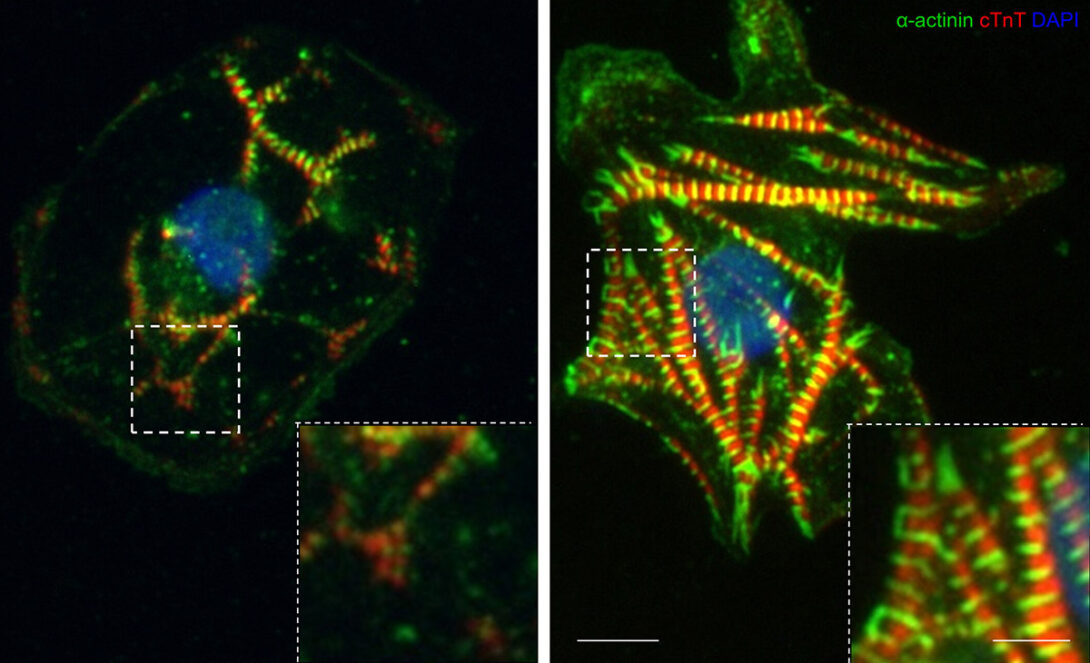
Researchers from the College of Medicine and the College of Engineering have developed a groundbreaking laboratory model that recreates the structure and activity of major cell types in the heart’s atrial chambers. The hope is that with this new model will come a better understanding of the irregular heart rhythm called atrial fibrillation which affects more than 30 million people globally, leading to stroke and heart failure in severe cases.
“This model is going to be incredibly useful for developing more effective personalized treatments for patients and for understanding atrial maturation,” said Dawood Darbar, MBCHB, MD, and chief of cardiology in the department of medicine. The model was co-developed by the research groups of Professors Darbar and Salman Khetani, PhD, who is faculty in the Richard and Loan Hill Department of Bioengineering and director of graduate studies in the college of engineering.
These groundbreaking discoveries and innovative technologies hold immense promise for improving the diagnosis and treatment of cancer and heart disease. As research continues, UI Health continues to offer access to excellent care and ground-breaking discoveries for our communities locally and afar.